General medicine assignment may 2021
Online monthly assignment for the month of May 2021
Name: B.Krishna
Roll no: 068
Batch: 2017
Semester: 8TH SEMESTER
I have been given the following cases to solve in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
This is the link of the questions asked regarding the cases:http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
Pulmonology
A.Link:
https://soumyanadella128eloggmr.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
1Q) what is the evolution of the symptomatology in this patient interms of an event timeline and where is the anatomical localisation for the problem and what is the primary etiology of the patient problem ?
1Ans)Evolution of symptomatology
20 yr back -1st episode of sob
12 yr back-2nd episode of sob
After that she has been having yearly episodes for the past 12 yrs
Diagnosed with diabetis - 8yrs back
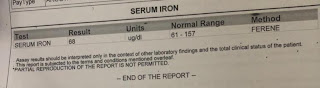
Anemia and took iron injections - 5yr ago
Generalised weakness - 1 month back
Diagnosed with hypertension - 20 days back
Pedal edema - 15 days back
Facial puffiness- 15 yrs back
Anatomical location of problem - lungs
Primary etiology of patient- usage of chulha continuously since 20 yrs m
2Q)what r the mechanism of action indication and efficacy over placebo of each of the phramacological and nonphramacological interventions used for this patient?
2Ans)Head end elevation :# MOA;
improves oxygenation
decreases incidence VAP
increases hemodynamic performance
increases end expiratory lung volume
decreases incidence of aspiration
2)Indication: head injury
meningitis
pneumonia
oxygen inhalation to maintain spo2
Bipap:non invasive method
1)MOA :assist ventilation by delivering positive expiratory and inspiratory pressure with out need for ET incubation9
3. Cause for current acute excerbation - it could be due any infection
4.could the ATT affected her symptoms if so how?
Yes ATT affected her symptoms
Isoniazid and rifampcin -nephrotoxic - raised RFT was seen
Cardiology
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
ANS:
Amount of blood pumped out of the heart with each beat is called the ejection fraction (EF). A normal EF is usually around 55 to 70 percent.
1)People with heart failure with reduced ejection fraction have an EF that is 40 to 50 percent or lower. This is also called systolic heart failure.
People with heart failure with preserved ejection fraction do not have much of a change in their ejection fraction. This is often called diastolic heart failure.
2)HFrEF were often diagnosed earlier in life and right after a heart attack.
HFpEF were diagnosed later in life and first experienced symptoms of heart failure between the ages of 65 and 70.Many of those with HFpEF also shared that they have other health problems that led to their diagnosis.
3)HFrEF shared that they feel depressed and/or anxious about their heart failure diagnosis. Risk factors for those in this group include genetics or a family history of heart failure.
HFpEF shared that they are still able to do the things they enjoyed before their heart failure diagnosis.risk factors, including:Sedentary lifestyle,High blood pressure,Sleep apnea&Other heart conditions
4)HFrEF are more likely to have had surgery, including surgery to implant a pacemaker or other heart rhythm control device.HFrEF shared that they currently use a combination therapy to treat their heart failure.
HFpEF have never had surgery to treat their heart failure or had a device implanted.
5)HFrEF are men who live in rural areas.
However, most respondents with HFpEF are women who live in urban areas.
2.Why haven't we done pericardiocenetis in this pateint?
ANS;
Pericardiocentesis is usually done when the pericardial effusion is not resolving on its own . Here the pericardial fluid which has accumulated was resolving on itw own , at the time of admission it was 2.4mm and when discharged it was 1.9 mm . Therefore we did not do pericardiocentesis in this pt.
3.What are the risk factors for development of heart failure in the patient?
ANS: IN THIS PATIENT:
NON MODIFICABLE RISK FACTORS:
age
gender
MODIFIABLE:
hypertension
smoking
type 2 diabetes .
kidney disease.
4.What could be the cause for hypotension in this patient?
ANS:The patient was anemic with Hb of 8gm/dl . One of the severe complication of anemia is tissue hypoxia which further lead to hypotension.
Link B:
https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-pedal.html
1.What are the possible causes for heart failure in this patient?
ANS:Causes of heart failure:
obesity
alcohol
diabetes
hypertension
2.what is the reason for anemia in this case?
ANS:
Alcoholics frequently have defective red blood cells that are destroyed prematurely, possibly resulting in anemia.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
ANS:
The pt. had recurrent blebs and ulcer on lower limbs (foot). This is due to Type 2 diabetes mellitus.
Diabetic foot ulcers generally arise as a result of poor circulation in the foot region. While high blood sugar levels and nerve damage or even wounds in the feet may result in foot ulcers in many cases.
There are many risk factors that may lead to foot ulcers at the end.
Poor quality or fitting of the footwear.
Unhygienic appearance of foot.
Improper care of the nails of the toe.
Heavy intake of alcohols and tobacco.
Obesity and Weight-related
Complication arising from Diabetes like eye problems, kidney problems and more.
Although aging or old age can also be counted among them.
4. What sequence of stages of diabetes has been noted in this patient?
ANS: alcohol------obesity------impaired glucose tolerance------diabetes mellitus------microvascular complications like triopathy and diabetic foot ulcer-------macrovascular complications like coronary artery disease , coronary vascular disease and peripheral vascular disease.
Link C:
https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
1Q) what is the evolution of the symptomatology in this patient interms of an event timeline and where is the anatomical localisation for the problem and what is the primary etiology of the patient problem ?
1Ans)Evolution of symptomatology
1st episode of sob - 20 yr back
2nd episode of sob - 12 yr back
From then she has been having yearly episodes for the past 12 yrs
Diagnosed with diabetis - 8yrs back
Anemia and took iron injections - 5yr ago
Generalised weakness - 1 month back
Diagnosed with hypertension - 20 days back
Pedal edema - 15 days back
Facial puffiness- 15 yrs back
Anatomical location of problem - lungs
Primary etiology of patient- usage of chulha since 20 yrs might be due to chronic usage
2Q)what r the mechanism of action indication and efficacy over placebo of each of the phramacological and nonphramacological interventions used for this patient?
2Ans)Head end elevation : MOA;
improves oxygenation
decreases incidence VAP
increases hemodynamic performance
increases end expiratory lung volume
decreases incidence of aspiration
Indication: .head injury
meningitis
pneumonia
oxygen inhalation to maintain spo2
Bipap:non invasive method
MOA :assist ventilation by delivering positive expiratory and inspiratory pressure with out need for ET incubation9
3. Cause for current acute excerbation - it could be due any infection
4.could the ATT affected her symptoms if so how?
Yes ATT affected her symptoms
Isoniazid and rifampcin -nephrotoxic - raised RFT was seen
Neurology
https://neerajareddysingur.blogspot.com/2021/05/general-medicine-case-discussion.html?m=1
1) What can be the cause of her condition ?
According to MRI cortical vein thrombosis might be the cause of her seizures.
2) What are the risk factors for cortical vein thrombosis?
Infections:
Meningitis, otitis,mastoiditis
Prothrombotic states:
Pregnancy, puerperium,antithrombin deficiency proteinc and protein s deficiency,Hormone replacement therapy.
Mechanical:
Head trauma,lumbar puncture
Inflammatory:
SLE,sarcoidosis,Inflammatory bowel disease.
Malignancy.
Dehydration
Nephrotic syndrome
Drugs:
Oral contraceptives,steroids,Inhibitors of angiogenesis
Chemotherapy:Cyclosporine and l asparginase
Hematological:
Myeloproliferative Malignancies
Primary and secondary polycythemia
Intracranial :
Dural fistula,
venous anomalies
Vasculitis:
Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
Link A:
https://kavyasamudrala.blogspot.com/2021/05/liver-abscess.html
Liver abscess
1Q)do u think drinking locally made alcohol cause liver abscess in this patient due to predisposing factors present in it ? What could be the cause in this patient?
1ans- yes, it could be due to intake of contaminated toddy
2Q)what is the etiopathogenesis of liver abscess in a chronic alcoholic patient?(since 30 yrs - 1 bottle/day)
2ans - according to some studies, alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess.
3Q)is liver abscess is more common in right lobe?
3ans-yes right lobe is involved due to its moreblood supply
4Q) what r the indications for usg guided aspiration of liver abscess
4ans- Indications for USG guided aspiration of liver abscess
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs

Comments
Post a Comment